Cervical cancer awareness
By Thandiwe Kubere
MASERU – With the rise of many life-threatening diseases, came a need for finding ways to protect, prevent as well as to treat ill-health. When health-care providers around the world sought ways of fighting the deadly virus causing cervical cancer around the globe, Lesotho was no exception. Health care providers in the country have travelled across communities and schools, giving the HPV vaccine to girls between the ages of 9 and 12.
Vaccinations have proved to be the most vital way of protecting oneself and their children against ill health. Studies reveal they prevent up to 3 million deaths worldwide every year. Vaccines teach the immune system how to create antibodies which protect from diseases. It has been said that once the immune system knows how to fight a disease, it is able to protect one’s body for many years and this is why vaccinations are important. As a result, it is much safer for the immune system to learn this through vaccination than by catching the diseases and treating them.
Women’s health expert Valentina Milanova, founder of Daye, a gynaecological health company enlightened that cervical cancer is the second deadliest cancer in women and assigned female at birth (AFAB) individuals.
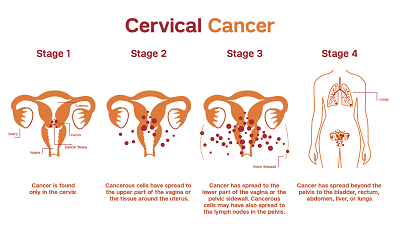
Mayo Clinic gynaecologic oncologist Kristina Butler describes cervical cancer as the abnormal growth of cells which starts in the cervix. Most cervical cancers are caused by various strains of the human papillomavirus, also called HPV. HPV is a common infection that is passed through sexual contact. When exposed to HPV, the body’s immune system typically prevents the virus from doing harm. However, in a small percentage of people, the virus survives for years, and this contributes to the process that causes some cervical cells to become cancer cells.
The cancer begins when healthy cells in the cervix change their DNA. A cell’s DNA contains the instructions that tell a cell what to do. The changes tell the cells to multiply quickly. In this case, the harmful cells continue living when healthy cells die as part of their natural life cycle. As a result, the cells then become too many and form a mass called a tumour. In time, the cells break away and spread to other parts of the body.
Moreover, HPV is a group of more than 150 related viruses that infect men and women. These common viruses infect about 13 million people, including teens, every year. Dr Emil Mchaki declared some HPV infections can lead to certain types of cancers. Therefore, the HPV vaccine protects against genital warts and most cases of cervical cancer. It protects against cancer of the vagina, vulva, penis or anus caused by HPV. It also protects against mouth, throat, head and neck cancers caused by HPV. The vaccine gives the body a safe way to build immune system awareness of some HPV strains. This means the body has an easier time clearing out those strains of the virus if a person catches them later.
“One can reduce their risk of developing cervical cancer by having screening tests and receiving a vaccine that protects against HPV infection”, he said.
When one suffers from cervical cancer, it is often first treated with surgery to remove the cancer. Other treatments may include medicines to kill the cancer cells. Options also include chemotherapy and targeted therapy medicines. Radiation therapy with powerful energy beams have also proven to be useful. Sometimes treatment combines radiation with low-dose chemotherapy, which on the other hand may inflict pain on the infected person as opposed to just as prickle when getting vaccinated.
Butler enlightened, when cervical cancer starts, it might not cause symptoms. However, as it grows, it might cause signs and symptoms such as: vaginal bleeding after intercourse, between periods or after menopause; menstrual bleeding that is heavier and lasts longer than usual; watery, bloody vaginal discharge that may be heavy and have a foul odour; pelvic pain or pain during intercourse.
To combat the deadly virus, the U.S. Food and Drug Administration (FDA) approved the Gardasil 9 vaccine (Human Papillomavirus 9-valent Vaccine) so that the dose could be administered to girls from the age of 9 and older. The Centers for Disease Control and Prevention (CDC) also approved this vaccine to be safe and effective. The vaccine was studied by thousands of people around the world, and these studies showed no serious safety concerns. Side effects reported in these studies were mild, including pain where the shot was given, fever, dizziness, and nausea. Vaccine safety continues to be monitored by CDC and the FDA.
The CDC suggests people younger than age 15 can be vaccinated with two doses, 6 to 12 months apart. The ideal age is before a person is sexually active. This is because once a person gets HPV, the vaccine may not be as effective. Another reason is that the vaccine’s goal is to prevent a new infection and if a person has the virus, the vaccine may not help the body clear out the virus. People who start the vaccine series later, at ages 15 through 26, should get three doses of the vaccine. These shots are given over six months.
The vaccine is less effective in preventing HPV-related disease in young women who have already been exposed to one or more HPV types. That is because the vaccine prevents HPV before a person is exposed to it. The HPV vaccine does not treat existing HPV infections or HPV-associated diseases.
On that note, studies have revealed risk factors for cervical cancer include: Smoking tobacco, this is because when HPV infections happen to people who smoke, the infections tend to last longer and are less likely to go away. Again, increasing number of sexual partner puts a person at a greater risk of getting HPV. Being sexually active at an early age also increases the risk of HPV and other sexually transmitted infections. Moreover, having other sexually transmitted infections, also called STIs, increases the risk. People with a weakened immune systems are also more likely to develop cervical cancer.
Therefore, to reduce the risk of cervical cancer, it is advisable to talk to health care providers about the HPV vaccine and get a dose to prevent the infection. It is also wise to get pap tests as this would detect precancerous conditions of the cervix. These conditions can be monitored or treated in order to prevent cervical cancer. Most medical organizations suggest beginning routine Pap tests at age 21 and repeating them every few years. Research suggests that vaccine protection is long-lasting. Current studies have followed vaccinated individuals for ten years, and show that there is no evidence of weakened protection over time.
Ultimately, getting young girls to vaccinate acts as a safe and advisable way of protecting their lives from the life-threatening cervical cancer.